Clinical research and medical practice both heavily rely on the placebo effect. It is a patient’s psychological reaction to using a fake medication, therapy, or operation. Even in the lack of an active medicinal ingredient, patients frequently claim improvements in their health or even symptom relief. This unusual event offers a significant avenue for further investigation in the field of medicine by implying that the mind may have more control over the body than previously believed.
Because it might induce favourable improvements in a patient’s condition because of the perception that they are receiving therapy, the placebo effect is significant. It creates a psychological basis upon which the transformational power of suggestion and conviction can work on bodily changes. This presents an alternative to the prevalent method of depending exclusively on pharmaceutical interventions, encouraging a comprehensive approach to patient care that considers psychological aspects as well.
Understanding the Concept of Placebos
Contents
Often called “sugar pills” or “dummy treatments,” placebos have no therapeutic efficacy at all. Despite their careful design to mimic actual medications or treatments, they are devoid of any active ingredients. Patients are guaranteed to feel as though they are receiving genuine treatment because the administration technique is typically the same as the actual treatment.
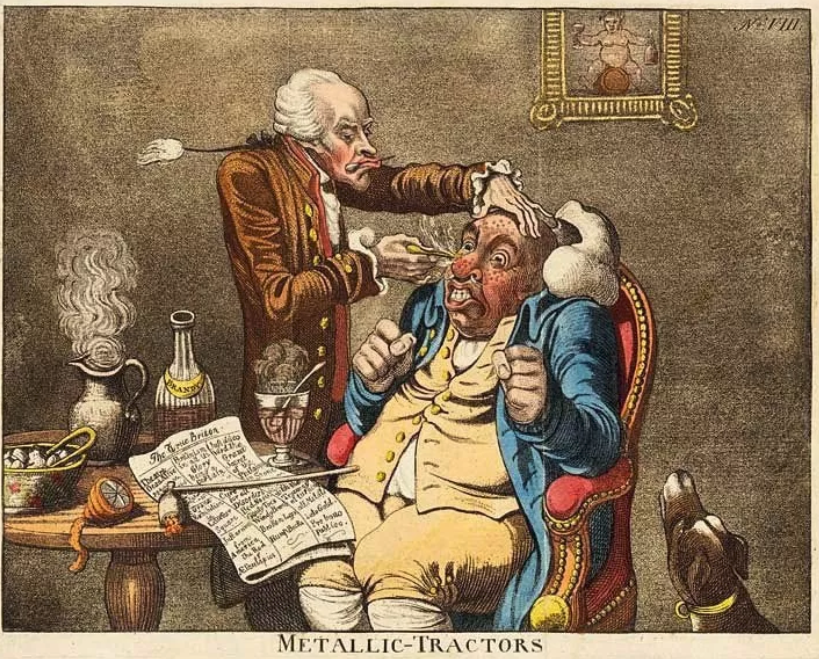
In the past, a treatment that a doctor administered primarily for the patient’s psychological well-being rather than any physiological benefit was referred to as a placebo. This practice dates back to the 18th century. But even back then, when healers employed symbols and rituals to elicit a healing response, the placebo effect was recognised and documented.
The placebo effect has been observed in various clinical and research settings, substantiating the concept that patient perception and belief can significantly affect treatment outcomes. In various instances, patients given a placebo have reported improvements in condition, from pain relief to reduced symptoms of depression, and even measurable changes like reductions in tumour size.
How Placebos Work
Complex psychological and physiological processes are involved in the mechanisms via which placebos function. A patient may develop a psychological expectation of improvement when they are given a placebo because they might think they are actually receiving a therapeutic drug or treatment. This anticipation sets off a chain of events in the brain that can resemble the effects of real medication or therapy.
To give an example, a patient with chronic pain might be treated with a placebo. The body’s natural painkillers, endorphins, may be released when the placebo is given because of a possible brain response. As a result, the patient may experience less pain and see an improvement in their condition. This illustrates how, even in the absence of therapeutic intervention, the placebo effect can improve patient outcomes.
Placebos have been used in a variety of treatments, frequently in double-blinded, randomised clinical trials. In these trials, the efficacy of novel treatments is assessed using placebos as the control group. On the other hand, placebos have also been used in routine clinical practice outside of this research setting. In situations where a patient’s expectations and beliefs are the primary determinants of their health outcomes, some doctors may employ placebo therapies.
The Science Behind Placebos
A combination of anthropology, psychology, and neurology underlies the science of the placebo effect. Numerous elements may be involved in the placebo effect, according to research. These include the care ritual, conditioning, cultural perspective, patient expectations, and the interaction between the patient and the practitioner.
Benefits of Placebos
The psychological effects of placebos are mostly responsible for their advantages. Since a placebo has no therapeutic value in theory, a patient’s belief and perception are the only factors that determine its effectiveness. Positive outcomes therefore emerge when patients’ faith in their treatment results in progress.

Pain management is among the most frequent applications of the placebo effect. In this case, a patient’s anticipation of pain alleviation may actually cause them to perceive less pain. This psychological phenomenon raises questions about the existing opioid crisis by implying that some pain problems can be treated without the need for highly addictive opioids.
In addressing mental health issues, the placebo effect may also be advantageous. One could argue, for example, that the placebo effect substantially explains the apparent effectiveness of antidepressants. This suggests that one important factor in the reduction of depression symptoms may be the belief and expectation of improvement.
Limitations of Placebos
Notwithstanding these possible advantages, there are certain moral and practical issues with the placebo effect. Informed consent is among the most important issues. A patient’s right to information regarding the nature and aim of any suggested therapy is fundamental to medical ethics. But telling people that a medicine is a placebo could make it less effective.

Nocebo effects, or adverse effects from placebo therapies, are also possible. This happens when a patient gets bad side effects because they were expecting bad reactions. For example, despite receiving a placebo, a patient who has been told that a medication may produce adverse effects such as nausea may nevertheless experience these effects because the medication does not contain any active ingredient that could cause them.
While it is tempting to see placebos as a cure-all, they cannot cure diseases or ailments but simply manage symptoms. Conditions that depend on physiological changes, such as infections or organ failure, cannot be treated effectively through the placebo effect.
The Current View and Future of Placebos
Modern perspectives on the placebo effect have moved beyond seeing it as a sham or merely a control in clinical trials. It is now recognized as a valid phenomenon that reflects the complexity of mind-body interaction in responding to healing and treatment. Understanding how placebos work is considered pivotal in enhancing patient care and the overall effectiveness of therapeutic interventions.

The use of placebos in the future may further refocus medical attention. When used, medical therapies could take a broader view, moving towards a more holistic strategy that integrates the mind’s role in health with the treatment of sickness. It is full of potential for developing novel therapeutic approaches, creating “open-label placebos,” and finding morally responsible ways to optimise patient benefit from benefits that were previously thought to be exclusively placebo-related.

